What is Periodontal Disease?
Periodontal disease is severe gum inflammation that if left untreated can lead to the loss of bone and tissue surrounds your teeth that inevitably leads to tooth loss over time. Periodontal disease stems from plaque buildup. You can prevent plaque buildup by brushing at least twice daily, flossing, and visiting your dentist twice a year for cleanings with the hygienist and exams with the doctor. Some symptoms patients experience with periodontal disease is bleeding and sore gums, bad breath, teeth that are mobile and gaps forming between teeth. If you are diagnosed with periodontal disease, we have the ability to help prevent future breakdown of gums and bone with scaling and root planning gum therapy and 3-month recare appointments. We will do all we can, with your help, to get you back stable oral foundation.
PERIODONTAL DISEASE
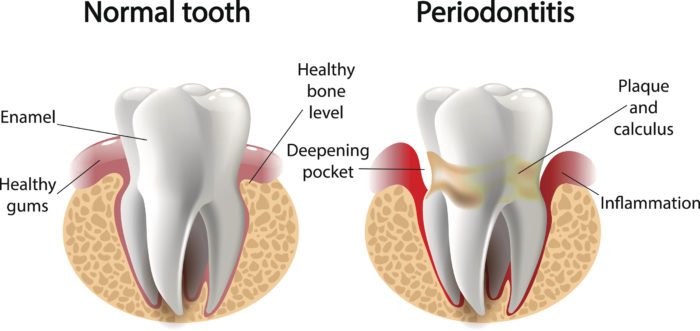
Periodontal disease is a term describing infection of the tissues which surround a tooth. There are two types of periodontal disease: ‘gingivitis’ is an infection and inflammation of the gums around the neck of a tooth whereas ‘periodontitis’ is an infection of the ligament and bone surrounding the root of a tooth.
Frequently Asked Questions
1. What causes Periodontal Disease?
Gingivitis occurs when plaque is allowed to build up around a tooth and create a sticky layer which causes a gum infection. If you look in your mouth you will see redness, swelling and bleeding of the gum around your tooth.
Periodontitis occurs in susceptible patients when a long-term gum infection is not treated. Infection and resultant inflammation lead to the loss of ligaments and bone around the root of your tooth.
Factors which significantly increase the risk of developing periodontitis include:
- Genetics
- Smoking
- Diabetes
- Medications (certain anti-seizure, blood pressure, and immunosuppressant medications)
- Stress
- Poor Oral Hygiene

2. What can I do to minimize my risk of Periodontal Disease?
To minimize your risk of future periodontal disease, you must be mindful of the risk factors stated above. Gingivitis is usually well managed by adopting excellent oral hygiene practices. Periodontitis is more difficult to manage.
Protocols recommended by your dentist may include:
Non-Surgical Periodontal Therapy
- Root cleaning (scaling and root planing) at the appropriate intervals to manage your risk for bone loss
- Antibacterial mouth rinses
- Oral antibiotics
- Customized home care instruction
- Smoking cessation counseling
- Surgical Periodontal Therapy
- Recontouring of gum and bone around affected teeth to allow better access for professional root cleaning and daily home care Surgical Periodontal Therapy
- Recontouring of gum and bone around affected teeth to allow better access for professional root cleaning and daily home care

3. How can an existing bite affect Periodontal Disease?
Bite problems on periodontally affected teeth can lead to accelerated periodontal disease and loosening of the teeth. If signs of a bite problem are present, the following may be considered to balance your bite and relieve excess pressure on periodontally involved teeth:
- Bite therapies including deprogramming and equilibration
- Orthodontic repositioning of the teeth
- Replacement of worn or damaged teeth
- Replacement of worn or damaged fillings
- Replacement of missing teeth
- Use of a custom-fitted bite guard to protect from grinding or clenching forces

4. What will happen if I choose to do nothing about my Periodontal Disease?
As uncontrolled periodontitis is progressive in nature, it will lead to increased bone loss and eventual tooth loss; ultimately affecting your ability to eat and speak. There are also connections between periodontal disease and other chronic diseases of the body such as cardiovascular disease, diabetes and rheumatoid arthritis. In pregnant women, periodontal disease is strongly linked to preterm, low birth weight.